About
Peristomal skin complications can occur from a wide variety of sources. Understanding the source can help target appropriate management strategies. Two of the most common sources are Peristomal Moisture Associated Skin Damage (PMASD) and Peristomal Medical Adhesive Related Skin Injury (PMARSI).
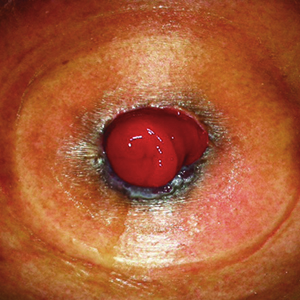
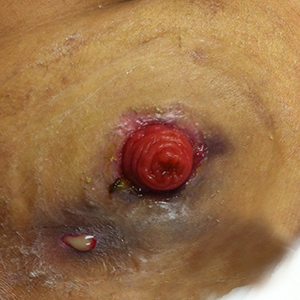
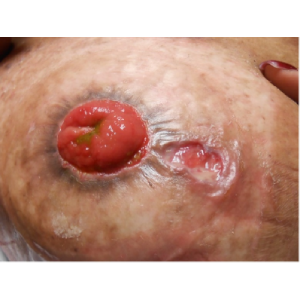
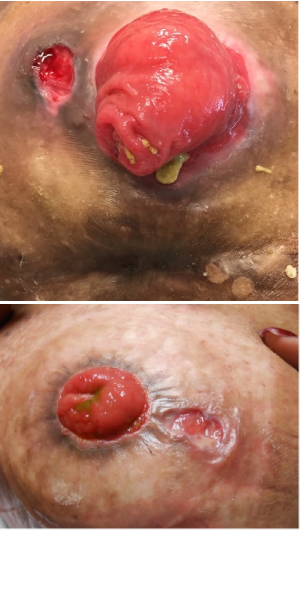
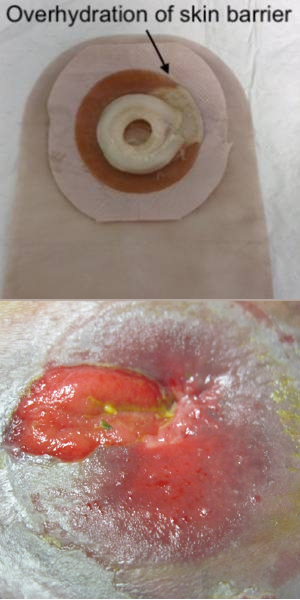
PMASD is defined as inflammation to the peristomal skin as a result of exposure to a moisture source such as urine or stool. Evolving terminology also uses the term irritant contact dermatitis (ICD) related to fecal or urinary stoma or fistula. Clinical experience also suggests that exposure to external moisture sources such as swimming, and the use of hot tubs, may also influence the presence of PMASD. This guide will help identify various PMASD sources including: irritant dermatitis, maceration, and fungal rash.
PMARSI is defined as erythema or other abnormal skin manifestations such as blisters, erosions or tears that persist for 30 minutes or more after removal of the adhesive. This guide will help identify various PMARSI sources including: folliculitis, and skin stripping (trauma).
Thank you to the original developers of the Peristomal Skin Assessment Guide:
Mikel Gray, PhD, FNP, PNP, CUNP, CCCN, FAANP, FAAN
Professor and Nurse Practitioner, Department of Urology,
University of Virginia, Charlottesville, Virginia
Janice C. Colwell, MS, RN, CWOCN, FAAN
Advanced Practice Nurse – Ostomy Care Services
University of Chicago, Chicago, Illinois
Dorothy Doughty, MN, RN, CWOCN, FNP, FAAN
Emory University Hospital, Atlanta, Georgia
Margaret Goldberg, MSN, RN, CWOCN
Clinical Nurse Specialist/WOC Nurse,
Delray Medical Center, Delray Beach, Florida
Jo Hoeflok, RN (EC), BSN, MA(LS), CETN(C), CGN(C)
Nurse Practitioner for Gastroenterology & General Surgery
St. Michael’s Hospital, Toronto, Ontario, Canada
Andrea Manson, RN, BSN, ET
Ostomy Care & Supply Centre,
New Westminster, British Columbia, Canada
Laurie McNichol, MSN, RN, CNS, GNP, CWOCN, CWON-AP, FAAN
Clinical Nurse Specialist/WOC Nurse,
Cone Health, Wesley Long Hospital, Greensboro, North Carolina
Samara Rao, BScN, RN, CETN(C)
Alberta Health Services Royal,
Alexandra Hospital, Edmonton Alberta, Canada
Joy Boarini, BSN, MSN, WOC Nurse
Hollister Incorporated, Libertyville, IL USA
Diane Owen, BSN, MBA
Hollister Incorporated, Libertyville, IL USA
Ginger D. Salvadalena, PhD, RN, CWOCN
Hollister Incorporated, Libertyville, IL USA
Karen Spencer, BN, ET
Hollister Incorporated, Libertyville, IL USA
The WOCN Society does not endorse any specific brands or products.